Common Ankle and Foot Conditions
Arthritis of the feet
Arthritis is a term used in medicine meaning inflammation of a joint. You have 26 bones and 13 joints in each foot so therefore, your foot and ankle are commonly affected by arthritis which can be characterized as:
• Pain during movement of the joints of the feet
• Tenderness in and around a joint
• Redness or swelling around a joint
• In severe cases, foot deformity as a result of prolonged arthritis
Certain types of arthritis such as rheumatoid arthritis, osteoarthritis, septic arthritis, gouty arthritis and psoriatic arthritis can present themselves in different ways, but the pain and complaint from the patient is similar. Many of these types can be identified on a simple radiograph taken while at your doctor’s appointment.
Ankle Sprain
The ankle joint is an important joint used for walking. A joint is formed where bones come together. Joints are held together by tissue called ligaments. The ligaments allow for motion of the bones at the joint, but only within certain ranges of motion.
An ankle sprain occurs when the ankle ligaments are stretched more than normal. This may be caused from the ankle “rolling” or “twisting” during an awkward fall or simply stepping down wrong. This may result in a partial tear or complete tear of the ankle ligaments.
The trauma to the ankle ligaments causes pain, bruising and problems bearing weight. The pain is usually located on the outside of the ankle but may cause pain to both sides of the ankle if severe. The ligament damage may result in the development of abnormal motion at the joint due to the loss of stability. This may increase the likelihood of future ankle sprains and instability of the joint which can lead to arthritic changes in the joint.
Athlete’s foot
Athlete’s foot is a fungal infection of the skin. Symptoms include itching and redness between the toes, peeling of the bottom of the foot and dry flaky skin.
Fungi can be found everywhere in the environment and athlete’s foot occurs when the immune system allow fungi to infect the skin. Those at higher risk are diabetic, immunocompromised people and those frequently exposed to areas where fungi like to live – such as public showers or baths.
Bunions / Tailor’s bunions
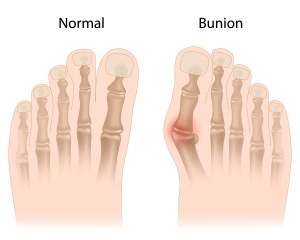
Bunions are often described as an enlarged bump on the side of the big toe. The visible bump actually reflects changes in the bony framework of the front part of the foot.
When bunions form, the big toe leans toward the second toe, rather than pointing straight ahead. This throws the bones out of alignment, producing the bunion’s “bump.”
Bunions are a progressive disorder. They begin with a leaning of the big toe, gradually changing the angle of the bones over the years and slowly producing the characteristic bump, which continues to become increasingly prominent. Usually the symptoms of bunions appear at later stages, although some people never have symptoms.
Tailor’s bunion, also called a bunionette, is an enlargement of the fifth metatarsal bone at the base of the little toe. The metatarsals are the five long bones of the foot. The enlargement that characterizes a tailor’s bunion occurs at the metatarsal “head,” located at the far end of the bone where it meets the toe. Tailor’s bunions are not as common as bunions, as described above, but both are similar in symptoms and causes.
The symptoms of bunions and tailor’s bunions include redness, swelling and pain at the site of the enlargement. These symptoms occur when wearing shoes that rub against the enlargement, irritating the soft tissues underneath the skin and producing inflammation.
Corns and calluses
Corns and calluses occur as the body’s way to protect itself from increased pressure.
Corns are thickened areas on top of the foot, usually the toes. Calluses are found on the bottom or sides of the foot. They often are due to improperly fitting shoes, such as shoes that are too tight or too narrow. However, they can also be due to foot deformities such as hammertoes and bunions.
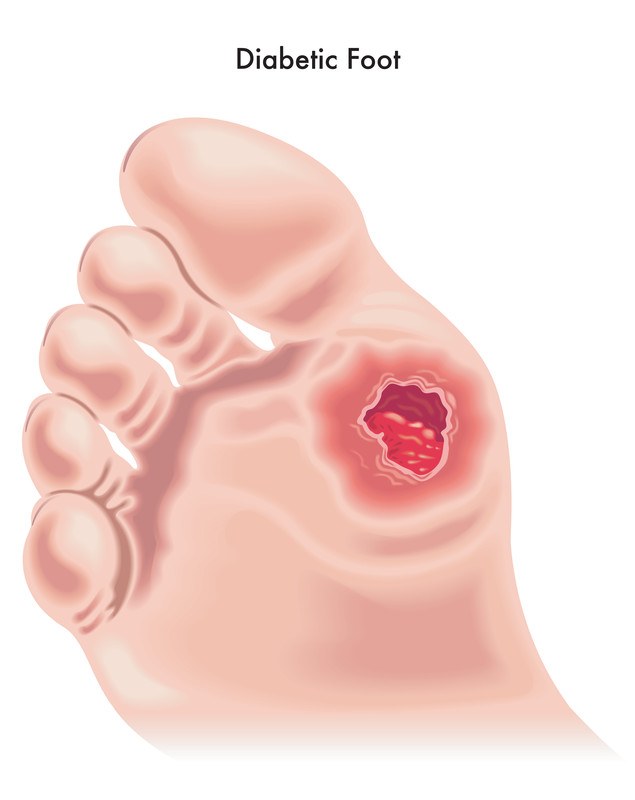
Diabetes-related foot problems

Diabetes can be dangerous to your feet, even a small cut could have serious consequences. Diabetes may cause nerve damage that takes away the feeling in your feet.
Diabetes may also reduce blood flow to the feet, making it harder to heal an injury or resist infection. An example of this would be not noticing a pebble in your shoe, so you develop a blister, then a sore, then a stubborn infection that might eventually lead to the amputation of your foot or leg.
To avoid serious foot problems that could result in losing a toe, foot, or leg:
• Inspect your feet daily. Check for cuts, blisters, redness, swelling, or nail problems. Use a magnifying hand mirror to look at the bottom of your feet. (If your eyesight is poor, have someone else do it for you.) Call your doctor if you notice anything.
• Moisturize your feet, but not between your toes. Use a moisturizer daily to keep dry skin from itching or cracking. But do not moisturize between the toes, as this could encourage a fungal infection.
• Cut nails carefully and straight across; file the edges. Don’t cut them too short, this could lead to ingrown toe nails.
• Wear clean, dry white socks and change them daily. Wearing white socks allows you to see at a glance if your feet might be bleeding.
• Shake out your shoes and inspect the inside before wearing. Remember, you may not feel a pebble, so always shake out your shoes before putting them on.
• Never walk barefoot – not even at home! You could step on something and get a scratch or cut.
• Take care of your diabetes. Keep your blood sugar levels under control. Keeping your blood sugar below 140 could decrease your chances of numbness and tingling in your feet.
• Never trim corns or calluses. No “bathroom surgery” – let your podiatrist do their job.
Get periodic foot exams. See your podiatrist on a regular basis for an examination to help prevent the foot complications of diabetes.
Flatfeet
Flatfooted is a term used to describe a foot where the arch appears to be non-existent when a person stands. Flatfooted patients tend to have pain at various areas of their feet, but mostly complain of pain at the instep or heel pain. These patients will also sometimes have impinging type pain at their outside ankle area. Patients will notice that most shoes are uncomfortable and do not provide the support needed.
Foot perspiration (excessive) and odor
The foot is densely covered with sweat glands, which causes excessive perspiration of the foot. This perspiration paired with wearing shoes and/or socks with inadequate air ventilation provides ideal conditions for bacteria and fungi to grow and thrive. Odor is the result of the growth of the bacteria and fungi. The excessive moisture contributes to athlete’s foot and plantar’s wart infections.
What can I do to prevent foot perspiration and odor?
• Thoroughly wash feet
• Choose properly fitting, cotton socks with proper ventilation. Many socks are made of nylon, which does not provide proper ventilation and increases perspiration, increasing foot odor.
• Change socks regularly
• Wear shoes only when necessary
See your doctor for a prescription topical medication
Foot ulcer
An ulcer is a sore on the skin or a mucous membrane caused by tissue breakdown. The ulcers that develop on feet are due to skin and tissue breakdown resulting in an open area.
Anyone can get ulcers on their feet, but it is more likely in someone who has decreased sensation in their feet. Although, diabetes is the most common cause of decreased sensation, or neuropathy, it can be caused by several conditions.
Ulcers usually develop over boney prominences and in areas of increased pressure. Once an area “breaks down” or becomes ulcerated you must decrease the pressure to that area for it to heal. This is caused by faulty biomechanics of your foot and ankle. Effectively healing ulcers requires adequate offloading, circulation, good nutrition and the prevention or management of infection. Only your foot and ankle specialists know the complicated biomechanics of your foot in order to heal your ulcer.
Foot and Ankle Fracture
Fractures are any break in the bones. It is usually due to fall or injury. Sometimes bone can break from overuse causing hairline fracture. These kinds of fractures are also know as Stress Fracture. Foot and ankle fractures are commonly misdiagnosed by Emergency room or Family Healthcare Providers due to subtly of the fractures. It is also important to know that fractures are not always easily seen on plain x-rays. MRI studies may be necessary to diagnose the fracture and the extent of the fractures. It is not always necessary to have surgery to fix a fracture. Only your specialists can determine based on the severity of the fracture what type of treatment is necessary. When fractures are not treated properly delayed union or non-union of the fracture can occur. This means that the bone at the fracture site may not heal without proper care. Your foot and ankle specialists may prescribe a bone stimulator or you may even need surgery to correct the problem.
Children can often break growth plates which are difficult to diagnose unless seen by foot and ankle specialists.
Hammertoes
A hammertoe is a toe that stays curled instead of being straight. This often makes the knuckle prominent and will become painful and rub on shoes. Sometimes due to the curling, all the weight is put on the tip of the toe and this area can become painful and callused as well.
Heel Pain
Heel pain is a very common complaint. You may have noticed a severe pain in the bottom of your heel, especially when you first step out of bed in the morning. You may also experience the pain after long periods of sitting. This pain is usually due to inflammation or irritation of a ligament that stretches from your heel bone to the ball of the foot, known as plantar fascia, and is called plantar fasciitis.
Heel pain may also be due to other causes such as a stress fracture, tendonitis, arthritis, nerve irritation or – less common – a cyst. Because there are several potential causes, it is important to have heel pain properly diagnosed.
What are the common causes of plantar fasciitis?
The most common cause of plantar fasciitis is usually due to a fault in the foot structure. If you are flatfooted or have high arches, you are more likely to develop plantar fasciitis. Also, wearing improper footwear on hard, flat surfaces can put a strain on the plantar fascia and lead to plantar fasciitis.
Call Now 239-481-7000
Ingrown toenail
An ingrown toenail is the result of the nail curving downward and growing into the skin, usually at the nail borders (the sides of the nail). This “digging in” of the nail irritates the skin, often creating pain, redness, swelling and warmth in the toe.
If an ingrown nail causes a break in the skin bacteria may enter and cause an infection in the area – often marked by drainage and a foul odor. However, even if your toe isn’t painful, red, swollen, or warm, a nail that curves downward into the skin can progress to an infection.
Metatarsalgia
Metatarsalgia is a term used to describe pain in the bottom of the ball of the foot while standing or walking. Sometimes patients will describe a burning or dull pain that continues to burn at the balls of the feet after resting. Patients will frequently say that it feels like they are walking on the bone and don’t have any padding in that area.
Since it is such a general term used to describe pain in the area, your physician will likely need xrays of your feet to rule out other problems or reasons why the pain is localized to that area.
Morton’s neuroma
A neuroma is a thickening of nerve tissue that may develop in various parts of the body.
The most common neuroma in the foot is a Morton’s neuroma, which occurs at the base of the third and fourth toes between the metatarsals. “Intermetatarsal” describes its location – in the ball of the foot between the metatarsal bones (the long bones extending from the toes to the midfoot).
Neuromas may also occur in other locations in the foot. The thickening, or enlargement, of the nerve that defines a neuroma is the result of compression and irritation of the nerve. This compression creates swelling of the nerve, eventually leading to permanent nerve damage.
Plantar warts
Plantar warts are skin growths on the soles or bottom of your feet. Their name comes from where they are located – plantar is the term used to indicate the sole of the foot.
These lesions or skin growths are caused by the human papillomavirus (HPV). This virus likely enters your body through tiny cuts and breaks in your skin.
Plantar warts often develop beneath pressure points in your feet, such as the heels or balls of your feet. A callus may build up over the wart as well. If the wart(s) develop under a pressure point, they may become painful and cause difficulty walking.
Prescription orthoses
Foot pain can often be alleviated with the use of prescription orthoses. These orthotics are designed from a custom impression of your feet. Our doctor evaluates biomechanics of your feet. Then takes an impression of your feet in a neutral position. The impression is then sent to a special lab to create personalized set of orthotics. They can be fabricated from several different materials making them more rigid or cushioned.
Custom prescription orthotics can be used to correct deformities or offload an area that is causing you pain. They can also be customized to allow your foot to function in the most efficient way possible decreasing unwanted movement.
Everyone from runners to the leisure walker can benefit from a pair of prescription orthotics.
Sports-related injuries
Sports injuries are unfortunately a common occurrence within the foot. Different sports such as soccer and track put added stress on the legs and feet and can lead to painful drawn-out injuries.
Frequently, injuries such as ankle sprains, muscle strains/tears, turf toe, fractures and dislocations are seen by podiatrists. Early diagnosis and clinical evaluation is a must for many of these injuries in order to avoid further injury.
Tendonitis
Tendonitis is simply means inflammation of your tendon. You feel pain and burning in the area of tendon and it’s usually due to decreased strength and flexibility. It is commonly due to every day activity but it can also lead to tendinitis.
Tendinosis is a little more serious problem. It is due to the generation of collagen in your tendon. It is slow to heal and usually end up not healing at all without any treatment. If you look at ultrasound images of the tendon you often see thickening of the tendon and it is because there’s partial tears.
Toenail fungus
The medical term for toenail fungus is onychomycosis, which means fungal infection of the nails. This condition may affect toe or finger nails, however toenail infections are particularly common. You may also experience pain in the toes and an odor from the nail fungus.
How do I know if I have toenail fungus?
Some common signs of toenail fungus are:
• Thickened and discolored nails, usually yellow
• Rough and crumbly nails that separate from the nail bed
• Nails that are distorted in shape
• A build-up of debris under the nail
How did I get toenail fungus?
Nail fungal infections are typically caused by a fungus that belongs to a group of fungi called dermatophytes. However, yeasts and molds can also be responsible. All of these microscopic organisms can be found anywhere, but prefer to live in warm, moist environments.
Toenail fungus is more common than fingernail fungus because your feet are often confined to a shoe, which provides the dark, warm and moist environment that fungi thrive in. Another reason is that the blood circulation at your toes is diminished when compared to your fingers, which may make it harder for your body’s immune system to fight off this infection.
When should I seek medical treatment for toenail fungus?
Nail fungus can be difficult to treat and once an infection begins it can persist indefinitely without medical intervention. See your podiartist at the first sign of nail fungus – often a tiny white or yellow spot under the tip of your nail.
Venous Insufficiency
Chronic venous insufficiency is a condition where blood pools in the veins of the lower legs.
The first signs of chronic venous insufficiency are usually ankle and leg swelling. Your legs may feel heavy, tired, itchy, or achy, especially at the end of the day or after prolonged standing.
As the swelling and pressure increases, your skin may actually start to leak a yellowish fluid from your pores. This fluid is plasma which is a normal component of blood.
Eventually, if the swelling is not stopped, the small blood capillaries will burst releasing red blood cells and giving the skin a reddish brown discoloration called hemosiderine. At this point the skin is very fragile which increases the chances of the patient to develop leg ulcers.
These ulcerations are called venous stasis ulcers and as with any opening in the skin, there is a high incidence of a secondary infection to the leg. This infection can spread very fast to the surrounding tissues and even become life threatening.
What causes chronic venous insufficiency?
Arteries bring oxygenated blood from the heart to the organs in the body and veins return the deoxygenated blood back to your heart and lungs. To accomplish this, blood needs to flow upward from the veins in the legs. For this to happen, the muscles in the lower extremities need to contract.This contraction will squeeze the veins, pushing the blood upward.
To keep the blood flowing in an upward direction and not back down, the veins contain one-way valves. This valve system is known as the venous pump and works very effectively when you walk, however when you sit or stand for long periods of time the blood in your legs can pool and increase the venous blood pressure.
Chronic venous insufficiency occurs when the valves in the vein become damaged and are not able to close all the way. This allows blood and fluid to leak backward causing blood to pool in the lower legs which is known as venous stasis.
Several things can cause the valves to be damaged including:
• Varicose veins
• Surgery
• Injury
• Obesity
• Missing valves in veins, or the valves in the veins do not work properly
• Blockage in the vein by a clot
• Muscles inadequately squeezing the veins